
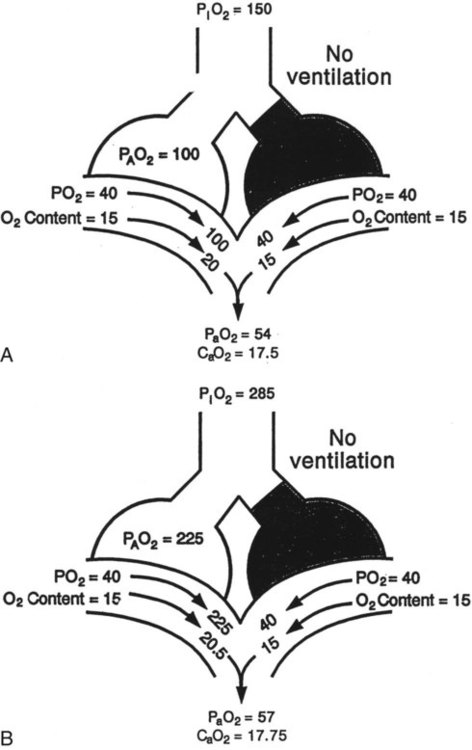
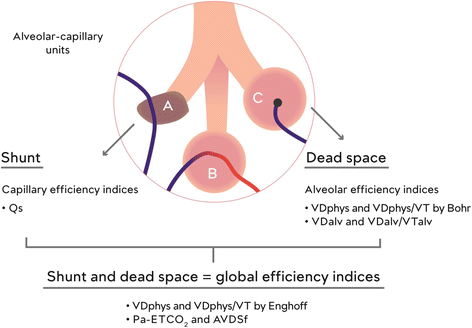
The perfusion of collapsed or consolidated lung units gives rise to intrapulmonary shunting and arterial hypoxemia, whereas the ventilation of non-perfused lung zones increases physiological dead-space, which potentially necessitates increased ventilation to avoid hypercapnia.Īrterial hypoxemia due to an intra-pulmonary shunt is a hallmark clinical problem. In patients with ARDS, disturbances in the physiological matching of alveolar ventilation (V) and pulmonary perfusion (Q) ( V/ Q mismatch) are a hallmark derangement. It is being increasingly demonstrated that the improvement of outcomes requires a tailored, individualized approach to therapy, guided by a detailed understanding of each patient’s pathophysiology. Acute respiratory distress syndrome (ARDS) remains an important clinical challenge with a mortality rate of 35–45%. Acute respiratory distress syndrome (ARDS) is a heterogenous condition that is characterized by the development of inflammatory pulmonary edema and life-threatening hypoxemia, and it accounts for nearly 25% of patients who require mechanical ventilation.


 0 kommentar(er)
0 kommentar(er)
